Now is doing time
Get ahead of the wave on COVID and other respiratory illnesses
Good news: the typical cold-weather wave probably has not yet arrived in Wisconsin. That’s my analysis of the most recent CDC data on COVID and other respiratory illnesses, anyway.
Mixed news: there are some parts of the state seeing high COVID transmission levels. And there are no guarantees that the respiratory wave won’t emerge — it’s just not here yet. Still, this gives Wisconsin faith communities time to stay ahead of the curve by implementing risk mitigation strategies.
What do we need to know?
Let’s do the numbers:
- Hospitalizations from COVID are down from a high at the end of September.
- So are wastewater levels. They’re still higher than anything we’ve seen since this spring, though.
- Wisconsin vaccination levels are pretty okay, actually. They’re not as high as the coastal cities, not as low as the South or Plains states. But for the most part, we’re doing as well as anyone when it comes to booster shots. More important, the levels of fully vaccinated and/or boosted senior citizens are quite high. That suggests Wisconsin’s health providers have made the vaccination case with the most vulnerable population.
Other respiratory disease levels, such as Influenza-Like Illnesses, currently fall into the “minimal” category, according to the CDC. (Wisconsin DHS hasn’t brought back its weekly report for the season.)
All of this fits national trends for both COVID and ILI. And all of it fits the idea that the cold-weather respiratory illness wave hasn’t arrived yet. We’ll see how the data look in a month or two.
There are of course some caveats to this picture:
- Our methods for tracking COVID aren’t great. The CDC relies on self-reporting from states, hospitals and other providers. If there isn’t reporting, or the reporting is late, the CDC tracking is off. Because of this, wastewater is considered the most reliable measure. However, a change in federal monitoring contracts means some data may fall through the cracks.
- Likewise, the CDC estimates COVID booster uptake, as they do with flu vaccines. I’m certainly not going to second-guess them, but it does add a layer of uncertainty into the reports. The CEO of Pfizer did estimate that around 17% of Americans would get the new boosters, about the same as last year. No word on his methodology, though.
So reports of COVID transmission are likely to be underestimates, not over. By how much? There’s no way to know.
That’s important, because some counties in Wisconsin fall into the CDC’s “High” category for hospital admissions. To wit: Iron, Vilas, Oneida and Forest, each of which has an admission rate of 21.7 per 100,000 residents.1. A handful of others are in the “Medium” class. That includes Barron, Chippewa, Waupaca, Outagamie, Calumet, Manitowoc and Sheboygan. We’re assuming we’ll see more of each category as we move from fall into winter.
What do we need to do?
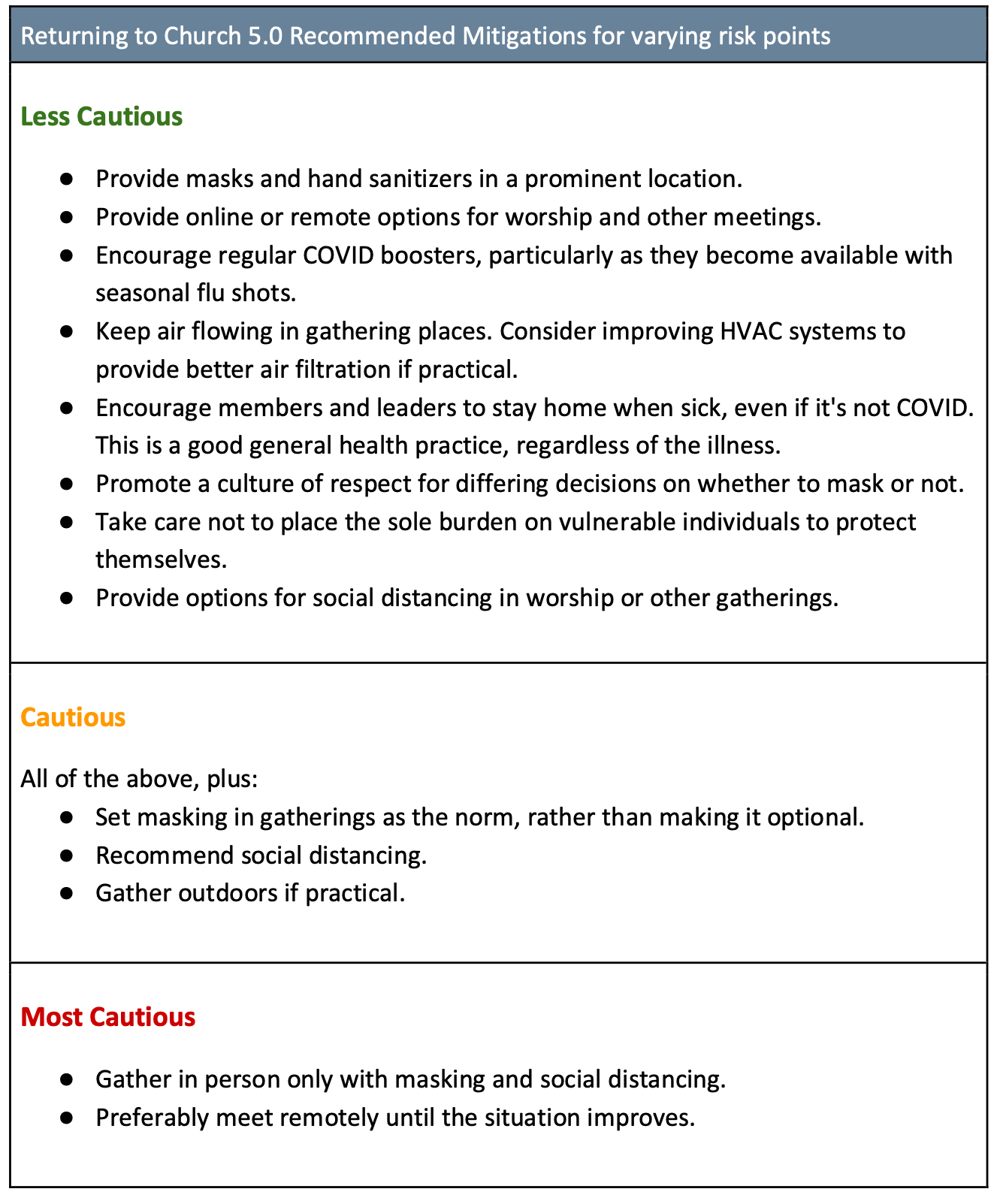
It’s difficult to map the new situation to the WCC’s Returning to Church guidelines. After all, we didn’t rely on hospital admissions when creating those guidelines. But let’s review the suggestions we laid out in Returning to Church 5.0:
We strongly suggest that everyone follow the practices in the “Less Cautious” bucket. Those are things we should all be doing, all the time, as a baseline for the new normal.
If you want to be proactive — and you do — go one level higher on our chart than the corresponding CDC guidelines. That is:
- If the CDC says your county is an area of low transmission, move up to “Cautious” in our guidelines.
- If you’re in a medium area according to the CDC, follow the practices in our “Most Cautious” level.
- Communities in high transmission areas should very much consider going back to remote gathering, especially those with many elderly or otherwise vulnerable members.
Remember: hospitalizations are a lagging indicator. COVID spreads most before hospital admissions peak. That means there’s a lot of incentive to take precautions before things appear to be the worst.
It’s possible that we won’t see much if any of a COVID wave this season. That would go against what we’ve seen in the past and current data, but COVID does continue to find ways to surprise us. So it could happen.
What if a wave is indeed developing? In that case, implementing mitigation protocols becomes more important each week. We’ve been suggesting that you talk about what measures your community should put into place. Now it’s time to do it, before it’s too late.
The Links
- Oh goody, #1: both A & B flu variants are circulating this year. That usually means we’re in for a more severe season. Now is the right time to get your booster!
- Oh goody, #2: health departments in Wisconsin and Illinois have reported measles cases. If you have not gotten your MMR vaccination and booster, please do.
- And Oh, goody #3: you’ve heard about food deserts, but how about pharmacy deserts? You might now, given that CVS, Walgreens and Rite Aid are all announcing store closures.
- Speaking of deserts, I love this quote: “For I was hungry and you ensured I did not live in a food desert, I was thirsty and you guaranteed my tap water was safe to drink, a stranger and your laws allowed me to find asylum, naked and your donation did not shame me, ill and you ensured I had affordable health insurance, in prison and the system rehabilitated me. – Fr. Michael Rozier, SJ, PhD., When Populations Become the Patient” (Tip o’ the pin to Kelly Moltzen)
- If you’re like me, you might have forgotten that Time magazine still exists. Yet here they are, with a useful guide on isolating after a COVID infection. Very short version: yes, you still need to isolate for five days after symptoms begin or a positive test. Then, mask in public for five days following isolation.
- Those Nerdy Girls have a nice guide to reducing the risk of infection at important events. It’s written more for meetings or reunions, but it can be applied to things like Christmas Eve services just as easily.
- Last but not least: new research suggests that depleted serotonin levels might be responsible for the brain fog seen in Long COVID patients. It’s a fascinating, brief read.