The hair on fire next time
Your survey answers about preparing for the next health emergency
Before I say anything else about the survey we fielded this spring and early summer, let me say thank you. We were able to collect 255 responses at last count. Some of those came through online forms, but the vast majority were interviews. The information we collected will help us plan the next phase of the Community Health Program.
Next, let me say thank you again to CHP Field Coordinator Angelica Espinoza. She was responsible for 131 of those interviews, either on her own or with her partner Angela Hicks. Angelica left the rest of us in the dust!
In all, we heard from 181 churches and 72 non-church partners. Of those, roughly 50 were Spanish-speaking respondents, and around 40 were African-American. About half of our responses came from outside the Milwaukee and Madison metro areas.
So we may not have collected a scientific sample, exactly. But I’m happy with the diversity of responses. And I think the results are close enough for horseshoes and hand grenades, as they say.1
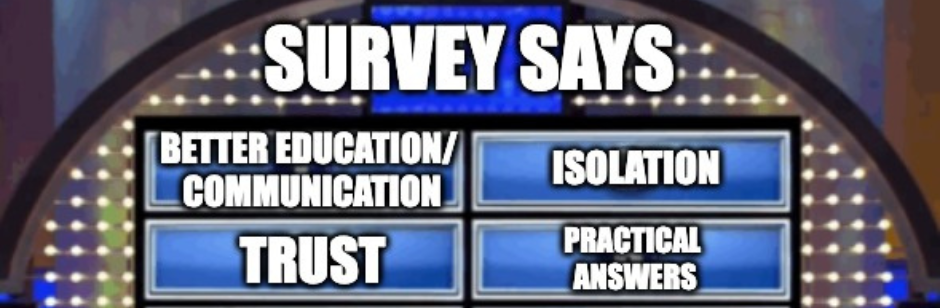
About those results: answers tended to cluster in a few different categories. Or so I thought, by my again unscientific review. Let’s look at each of them in turn.
Better Education/Communication
This was our largest single area of response. Many people we spoke with pointed to a need for better education around COVID, vaccines, and the need for risk mitigations. A number talked about how this information failed to register with different populations: young people, residents of nursing homes, members of Black churches.
Interviewees were not happy with the way anyone communicated with anyone:
-
- Political leaders
- Medical and public health officials
- Media and social media
- Church leaders
- Church members
- Society at large
We heard complaints about all of them. And yes, at least one person said WCC guidelines should have been more directive. “When the WCC said ‘We can’t tell you what to do’ it wasn’t helpful,” according to her. That was an admittedly uncharacteristic response. More people talked about wanting flexible responses to the pandemic, tailored to local concerns.
For the most part, however, responses focused on getting reliable information to the public and doing a better job of coordinating efforts.
Trust
Public health information did not connect with a significant part of the population. Most of the people we talked wanted better communication about the pandemic. Some saw a need to build trust in science, in public health, or in general. We also talked to a few skeptics who mentioned their inability to trust information about COVID.
Misinformation, Division & Politics
Respondents were very clear about what they considered the source of mistrust. “I’d shut off social media [next time] because politicians now have a voice to spread misinformation,” said one.
Again and again we heard that politics needed to be taken out of public health. People told us that politics created misinformation and disinformation, that politics sponsored divisions and prevented a united front in response to COVID.
One pastor objected to asking what communities should do to prepare. “The question should really be ‘What do legislators need to be prepared?'” he said. In his opinion, creating better ways to keep politicians accountable would improve pandemic response.
Some responses mentioned internal church politics. Some cited a need for cultural change to tamp down partisan divisions and strengthen communities.
Isolation and Health
Many people argued for stricter adherence to safety guidelines. Others worried that social distancing harmed mental, physical and spiritual health. Some would have reduced or done away with distancing altogether. Most seemed to be looking for ways to offset necessary sacrifices.
Not surprisingly, isolation affected communities in different ways. Hispanic/Latine pastors pointed to social distancing interfering with their parishioners’ employment. White congregations spoke about losing emotional support or the closeness in community. All groups recommended developing ways to maintain in-person connection while observing safety precautions.
Only a handful of interviewees (8) said their primary response to a new pandemic would be to provide spiritual care to their community. More (9) argued in favor of increased mental health services. Almost everyone understood the role of their organization to be primarily social.
Practical Answers
Many respondents had practical suggestions to offer. Improving access to health care and increasing financial supports during a pandemic were popular answers. One person noted that health care in El Salvador is free. Planning ahead was a common response, as was advocacy or grassroots organizing.
Other answers included:
-
- Focusing on youth
- Finding ways to collaborate or break out of silos between churches, community groups, schools and government agencies.
- Increased funding for public health.
- Repealing laws that prevent undocumented immigrants from acquiring a driver’s license or state ID. Those regulations seem to have interfered with their getting vaccines.
- Expanding response capability on a local level through interagency cooperation, fully staffed public health centers, or more community health workers.
- Doing more preventive work to improve general health
One individual offered an intriguing suggestion:
I would like to see a consistent platform for people of color to discuss important issues affecting our community on the daily including public health issues.
That’s quite right, and actually applicable to everyone. We don’t have great ways in our society to talk through important issues affecting our communities. And yes, that includes public health. The gaps and divisions that prevent us from having those conversations prevent us from taking meaningful, transformative action on the issues. That in turn leaves us vulnerable to another confused, conflicted, compromised response to the next big emergency. We need to do something about that.
The Links
- The CDC has begun tracking a new COVID variant. So far it doesn’t seem to be a big worry, but apparently they think it’s worth keeping an eye on.
- Why aren’t kids getting all their vaccines?
- Some useful information on the new OTC birth control medication from our friends at Those Nerdy Girls. (Seriously: it mentions drawbacks and limitations, among other things.)
- The Wisconsin Area Health Education Center in Milwaukee is offering trainings for community health workers or people interested in becoming one.
- Scent dogs have been trained to detect people with COVID infections, even pre-symptomatic and asymptomatic individuals. That really should have been the focus of today’s newsletter, to be quite honest.